Scale up Mpox Response, Health Groups Urge
Health Activists and Organizations Urge an Intensified Response to the Mpox Outbreak in Africa
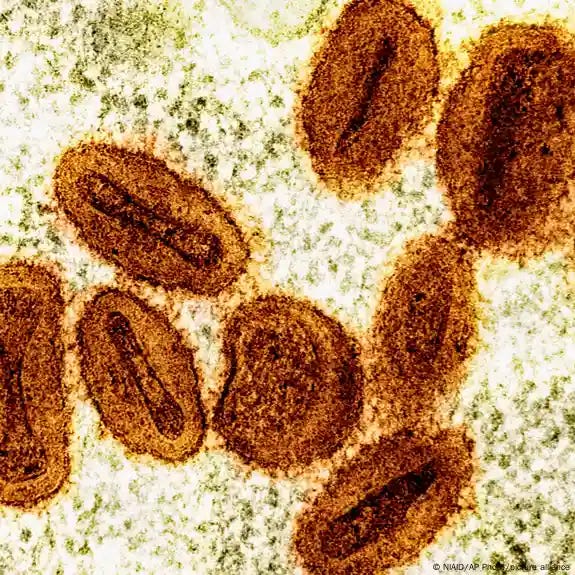
Thousands of people across Africa have been infected with the Mpox virus, resulting in hundreds of deaths and the ongoing spread of the disease. In response, over 55 health groups have urged the British government to support health systems in the affected countries.
In an letter circulated on 23 August, the groups demand rapid distribution of vaccines to countries in Africa currently struggling with mounting a response to the outbreak, as well as ensuring sharing of technologies between existing vaccine producers and manufacturers in Africa to increase global supply.
Dire situation in DRC
Elia Badjo, a medical doctor and global health expert with COSAMED, a health providers’ association in the Democratic Republic of the Congo (DRC), is among the signatories of the letter. In a conversation with People’s Health Dispatch, Badjo detailed the challenges the country faces due to the Mpox outbreak, including shortages of vaccines and testing capacities.
Speaking from South Kivu, one of the regions hardest hit by the crisis, Dr. Badjo highlights that health workers can only confirm about half of the suspected cases through testing. He emphasizes that without adequate testing capacities, responders are unable to accurately determine the true number of infections.
Even without full confirmation, it’s known that approximately 95% of Mpox cases in this outbreak are in the DRC. The country has reported around 14,000 cases and 500 deaths, while struggling with unequal access to treatment. In South Kivu, only 11 out of 29 affected health zones have treatment capacities, and many lack proper isolation facilities. Contact tracing remains a “real challenge,” as Dr. Badjo highlighted in a statement accompanying the open letter.
The DRC was heavily affected by previous Mpox outbreaks, including the one in 2022 which was declared a public health emergency of international concern by the World Health Organization (WHO). When the WHO declared the end of that global outbreak in 2023, infections were still circulating in the DRC, but no plans were made to prepare for the current resurgence, says Mohga Kamal-Yanni, Policy Co-Lead at the People’s Medicines Alliance.
Dr. Badjo notes that while the DRC had previously developed a national plan to address Mpox, it struggled with consistent implementation. Translating lessons from past outbreaks into effective policy has been challenging at least. Nevertheless, Dr. Badjo believes that there are short- and medium-term measures that can enhance the response, such as expanding community mobilization efforts. “Community resistance should be fostered and strengthened,” he emphasizes.
Persistent problems with vaccine availability
A major issue is the limited availability of vaccines, which are produced by only a few private manufacturers and sold primarily to high-income countries at around USD 100 per dose. Most of these vaccines end up in the United States and Europe, bypassing regions like Africa, where Mpox has been a reality for decades. In severe outbreaks, these countries typically donate a small portion of their reserves to affected regions, leaving a significant gap in vaccine accessibility.
The current situation is similar. Japan has pledged 3 million vaccine doses for the Mpox response, while the US and European countries have committed tens of thousands of doses. However, this falls far short of what is needed. The DRC alone estimates it requires 4 million doses for its response efforts, while the Africa Centers for Disease Control and Prevention (Africa CDC) projects that 10 million doses are necessary to address the current outbreak.
Even if all existing production capacities were fully dedicated to delivering vaccines where they are urgently needed, a significant shortfall would likely remain. Recently, existing producer Bavarian Nordic announced that it could produce up to 10 million doses—but only by the end of 2025.
In this context, the letter argues, decentralizing production is essential. “Every day counts when it comes to public health emergencies; it is about meeting the demand as soon as possible to prevent the spread of the disease. If manufacturers on the continent can make doses, you will meet the demand faster,” says Jake Atkinson, Senior Campaigns and Media Advisor at STOPAIDS.
“Long-term, we need to support local production of health tools in all parts of the world otherwise we will lack the capacity to respond to future pandemics or emergencies.”
Launching vaccine production in Africa would require significant effort, explains Kamal-Yanni. Success would hinge on current manufacturers agreeing to technology transfers, including both knowledge and physical infrastructure, and ensuring that local companies receive sufficient financial and logistical support. With these conditions met, there are producers in Africa capable of taking on the task, Kamal-Yanni asserts.
Problems extend beyond access to vaccines
African countries grappling with Mpox face challenges beyond vaccine shortages, including weakened cold chain logistics and limited testing capacities. Atkinson points out that while these issues are complex, there are steps that high-income countries, such as the UK, can take to help address them.
“Many countries are spending more on debt repayments than their own public health budgets, which is utterly unsustainable. Countries must support debt restructuring and where possible debt cancellation in order for low- and middle-income nations to invest in their own health systems,” he says.
Kamal-Yanni highlights that addressing the root causes of these issues requires collaboration between governments from both the Global South and North. She stresses that healthcare must become a global priority with appropriate long-term funding, particularly for health systems and agencies like the WHO and Africa CDC. While surveillance is widely discussed, she notes that it is often disregarded that effective health surveillance demands skilled personnel and proper equipment, which requires dedicated funding.


